Demystifying Acid Reflux Disease: Causes, Symptoms, Diagnosis, and Treatment
Demystifying Acid Reflux Disease: Causes, Symptoms, Diagnosis, and Treatment
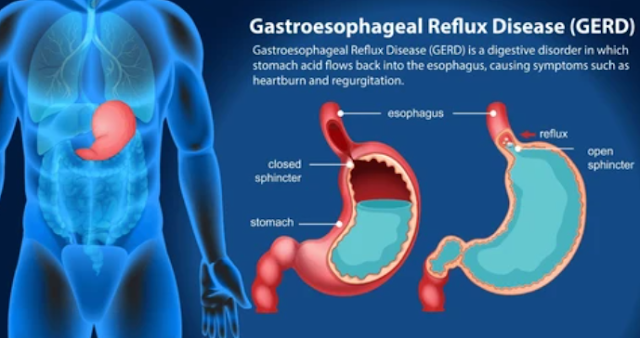
Acid reflux disease, also known as gastroesophageal reflux disease (GERD), is a common and chronic condition that affects millions of individuals worldwide. It is characterized by the regurgitation of stomach acid into the esophagus, causing a wide range of uncomfortable symptoms. While acid reflux disease may not be life-threatening, it can significantly impact a person's quality of life and lead to complications if left untreated. In this comprehensive article, we will explore the various aspects of acid reflux disease, including its causes, symptoms, diagnosis, and treatment options, to provide a deep understanding of this prevalent condition.
I. Understanding Acid Reflux Disease
To comprehend acid reflux disease fully, it is essential to differentiate it from occasional acid reflux or heartburn. Acid reflux becomes a disease when it occurs regularly or causes complications.
1. Occasional Acid Reflux vs. Acid Reflux Disease
Occasional acid reflux, commonly referred to as heartburn, is a normal and typically infrequent occurrence for many individuals. It may result from overeating, consuming certain foods, or lying down shortly after a meal. In contrast, acid reflux disease, or GERD, involves chronic and recurring episodes of acid reflux that cause significant discomfort or complications.
2. The Role of the Lower Esophageal Sphincter (LES)
The lower esophageal sphincter (LES) plays a pivotal role in the development of acid reflux disease. This muscular ring located between the esophagus and the stomach acts as a valve, preventing stomach acid from flowing back into the esophagus. In cases of GERD, the LES becomes weakened or relaxed, allowing stomach acid to reflux into the esophagus.
II. Causes and Risk Factors
Understanding the causes and risk factors of acid reflux disease is crucial for both prevention and effective management.
1. Weak Lower Esophageal Sphincter (LES)
A weakened LES is the primary cause of acid reflux disease. Factors contributing to LES dysfunction include obesity, smoking, and genetic predisposition. Pregnancy can also weaken the LES due to increased abdominal pressure.
2. Dietary Factors
Certain foods and beverages can exacerbate acid reflux symptoms. These include spicy foods, fatty or fried foods, citrus fruits, tomatoes, chocolate, caffeine, and alcohol. Identifying and avoiding these trigger foods can help manage the condition.
3. Obesity
Excess body weight, especially in the abdominal area, increases intra-abdominal pressure, pushing stomach contents, including acid, into the esophagus. Obesity is a significant risk factor for acid reflux disease.
4. Smoking
Smoking weakens the LES and reduces saliva production, which normally helps neutralize stomach acid. Quitting smoking is not only beneficial for overall health but can also improve acid reflux symptoms.
III. Common Symptoms of Acid Reflux Disease
Acid reflux disease can manifest through a range of symptoms, which may vary in severity from person to person.
1. Heartburn
Heartburn is the hallmark symptom of acid reflux disease. It is characterized by a burning sensation in the chest, often radiating towards the throat. Heartburn typically occurs after meals or when lying down and can last from a few minutes to several hours.
2. Regurgitation
Regurgitation involves the involuntary flow of stomach contents, including acid, into the mouth or throat. This can lead to a bitter or sour taste and discomfort.
3. Chest Pain
Chest pain related to acid reflux disease may mimic the symptoms of a heart attack. It is essential to differentiate between the two, as chest pain due to GERD is typically not associated with exertion and is relieved by antacids.
4. Difficulty Swallowing (Dysphagia)
In more severe cases of acid reflux disease, inflammation and damage to the esophagus can lead to difficulty swallowing. This is known as dysphagia and may require medical attention.
5. Chronic Cough and Hoarseness
Acid reflux can irritate the airways, leading to a chronic cough or hoarseness, especially in the morning.
IV. Complications of Acid Reflux Disease
Left untreated, acid reflux disease can lead to various complications, some of which can be serious or even precancerous.
1. Esophagitis
Recurrent exposure to stomach acid can cause inflammation of the esophagus, known as esophagitis. This condition can result in pain, difficulty swallowing, and the formation of ulcers.
2. Barrett's Esophagus
Barrett's esophagus is a precancerous condition that can develop as a consequence of long-term acid reflux. It involves changes in the cells lining the lower esophagus and carries an increased risk of esophageal cancer.
3. Esophageal Strictures
Repeated injury to the esophagus can lead to the formation of scar tissue, resulting in narrowed areas known as strictures. This can make swallowing difficult and may require dilation procedures.
4. Respiratory Complications
Acid reflux can lead to respiratory problems, including asthma exacerbations, chronic cough, and recurrent pneumonia, as stomach acid can enter the airways.
V. Diagnosis and Medical Evaluation
When acid reflux symptoms become chronic or severe, seeking a medical evaluation is essential. A healthcare professional, typically a gastroenterologist, can provide an accurate diagnosis and determine the appropriate course of treatment.
1. Clinical Assessment
During a clinical assessment, the healthcare provider will review the patient's medical history, including their symptoms, dietary habits, and lifestyle factors. This information helps identify potential triggers and risk factors for acid reflux disease.
2. Upper Endoscopy
Upper endoscopy is a procedure that involves the insertion of a flexible tube with a camera (endoscope) through the mouth to examine the esophagus, stomach, and upper part of the small intestine. It allows the healthcare provider to assess the severity of esophageal damage, identify complications, and obtain tissue samples if necessary.
3. Ambulatory pH Monitoring
Ambulatory pH monitoring involves the placement of a small tube through the nose into the esophagus to measure acid levels over a 24-hour period. This test helps confirm acid reflux and assess its frequency and severity.
VI. Treatment Options for Acid Reflux Disease
Treatment for acid reflux disease aims to alleviate symptoms, heal esophageal damage, and prevent complications. The choice of treatment depends on the severity of the condition and individual factors.
1. Lifestyle Modifications
- a. Dietary Changes: Identifying and avoiding trigger foods and adopting a GERD-friendly diet can reduce symptoms.
- b. Weight Management: Achieving and maintaining a healthy weight can significantly improve acid reflux symptoms, as excess abdominal fat increases pressure on the stomach.
- c. Elevating the Head of the Bed: Raising the head of the bed by 6-8 inches can help prevent nighttime acid reflux by allowing gravity to keep stomach acid down.
2. Over-the-Counter (OTC) Medications
- a. Antacids: Antacids, available without a prescription, can provide immediate relief by neutralizing stomach acid. They are suitable for occasional heartburn.
- b. H2-Receptor Antagonists (H2 Blockers): Over-the-counter H2 blockers like ranitidine or famotidine reduce acid production and are suitable for mild to moderate GERD symptoms.
3. Prescription Medications
- a. Proton Pump Inhibitors (PPIs): PPIs, such as omeprazole, esomeprazole, and lansoprazole, are potent acid reducers and are prescribed for moderate to severe acid reflux disease. They are typically taken once daily before breakfast.
- b. Prokinetics: Prokinetic medications help strengthen the LES and promote better stomach emptying. They may be prescribed in combination with other medications for certain cases.
4. Surgical Interventions
- a. Fundoplication: Fundoplication is a surgical procedure that involves wrapping the top of the stomach around the LES to strengthen it and prevent acid reflux.
- b. LINX Device: The LINX device is a small, flexible band of magnetic beads implanted around the LES to prevent acid reflux while allowing food to pass through.
- c. Endoscopic Procedures: Endoscopic therapies, such as transoral incisionless fundoplication (TIF) and radiofrequency ablation (Stretta), are minimally invasive options that can strengthen the LES and improve symptoms.
5. Barrett's Esophagus Management
Patients with Barrett's esophagus require regular surveillance endoscopy to monitor for dysplasia or cancer. In some cases, treatments like endoscopic mucosal resection (EMR) or radiofrequency ablation (HALO) may be necessary to remove or destroy abnormal tissue.
VII. Lifestyle Tips for Managing Acid Reflux Disease
In addition to medical treatment, adopting certain lifestyle changes can significantly improve acid reflux disease management.
1. Eating Habits
- a. Smaller, More Frequent Meals: Eating smaller portions and spreading meals throughout the day can reduce pressure on the LES.
- b. Chew Thoroughly: Chewing food slowly and thoroughly can ease digestion and reduce the risk of swallowing excess air, which can contribute to acid reflux.
- c. Avoid Eating Close to Bedtime: Finish eating at least two to three hours before lying down or going to sleep.
2. Dietary Choices
- a. Avoid Trigger Foods: Identify and avoid foods that trigger acid reflux symptoms. Common triggers include spicy foods, citrus fruits, tomatoes, caffeine, and chocolate.
- b. GERD-Friendly Diet: Consider adopting a GERD-friendly diet that includes lean proteins, non-citrus fruits, vegetables, whole grains, and low-fat dairy products.
3. Posture and Sleep
- a. Sleep Position: Elevate the head of your bed by 6-8 inches or use a wedge pillow to prevent nighttime acid reflux.
- b. Avoid Bending Over: After eating, avoid bending over or lying down, as this can increase the risk of acid reflux.
4. Smoking Cessation
Quitting smoking can significantly improve LES function and reduce the frequency and severity of acid reflux.
5. Stress Management
Stress can exacerbate acid reflux symptoms. Incorporating stress-reduction techniques such as yoga, meditation, or deep breathing exercises can be beneficial.
VIII. Conclusion
Acid reflux disease, or GERD, is a common and chronic condition characterized by the regurgitation of stomach acid into the esophagus, leading to uncomfortable symptoms and potential complications. While it may not be life-threatening, acid reflux disease can significantly impact a person's quality of life if left untreated. Understanding the causes, symptoms, diagnosis, and treatment options is essential for effectively managing this condition.
Treatment approaches range from lifestyle modifications and dietary changes to over-the-counter and prescription medications, and in severe cases, surgical interventions. The choice of treatment depends on the severity of the condition and individual factors.
By adopting a combination of medical treatment and lifestyle changes, individuals with acid reflux disease can find relief, reduce symptoms, and prevent complications. Regular medical evaluation, especially for those with chronic or severe symptoms, is crucial for effective management and prevention of long-term complications like Barrett's esophagus or esophageal cancer.
Ultimately, by demystifying acid reflux disease and raising awareness of its causes and management strategies, we can empower individuals to take control of their health and improve their overall quality of life.